Diamond Blackfan Anemia (“DBA”) is a rare blood disorder characterized by a failure of the bone marrow.
What is DBA Syndrome?
Diamond Blackfan Anemia (DBA) syndrome was first recognized as a distinct entity in 1938, although it was called “congenital hypoplastic anemia” by Dr. Louis K. Diamond and Dr. Kenneth D. Blackfan. Until recently, DBA syndrome was simply “DBA.” Due to the variability of symptoms between patients, individuals presenting with a known genetic mutation but without the typical features, and individuals being diagnosed in adulthood, the medical community decided to expand the name to Diamond Blackfan Anemia Syndrome. This new name intends to capture all patients with DBA syndrome.
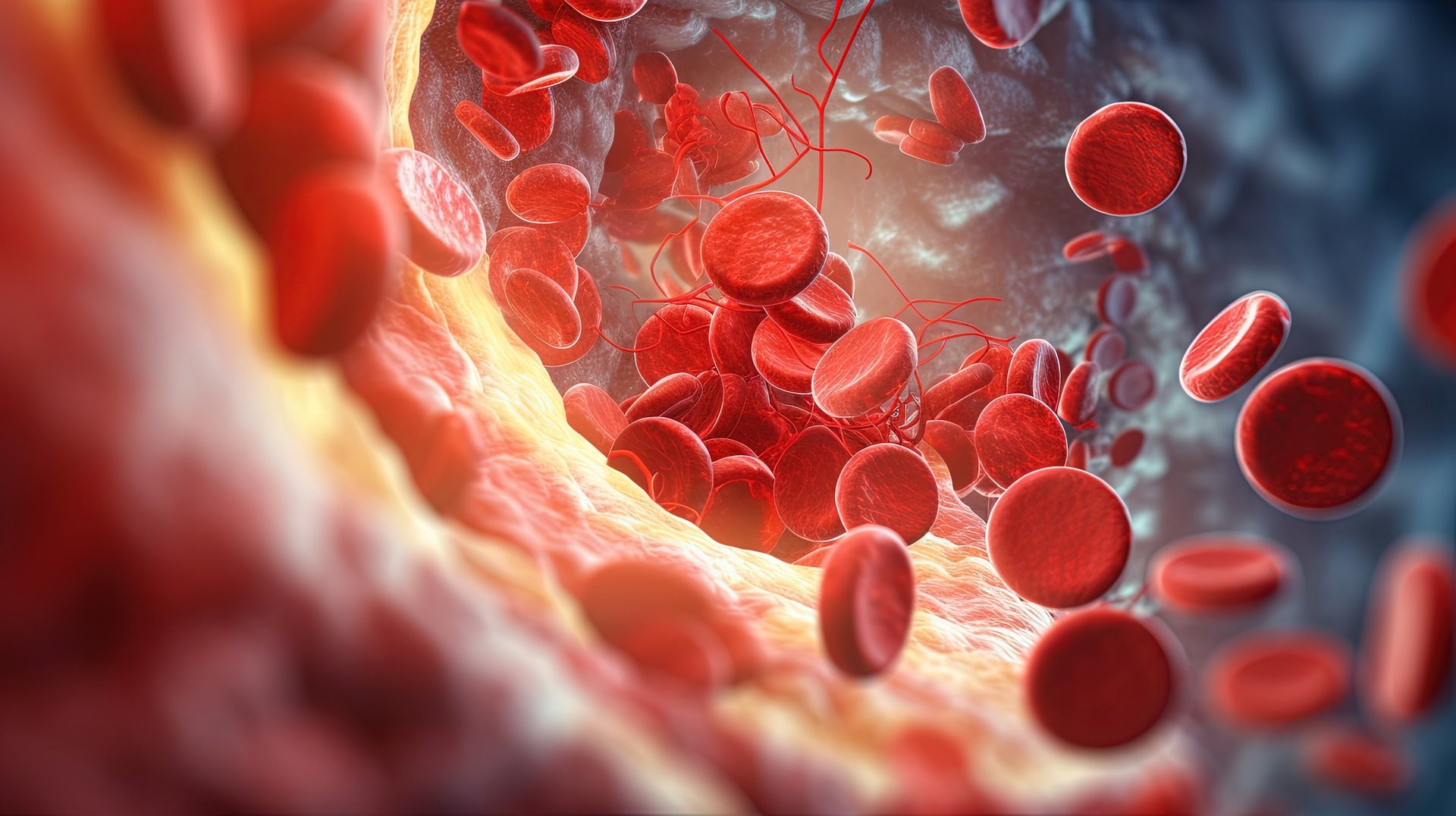
DBA syndrome is a rare inherited bone marrow failure syndrome, most often characterized by a failure of the bone marrow to produce red blood cells. This failure causes severe anemia, which is quite different from anemias caused by deficiencies in iron, vitamin B12, folate (folic acid), or erythropoietin. Some DBA syndrome patients may also have low neutrophils, low platelets, immunodeficiencies, and congenital abnormalities. Others may not exhibit any symptoms and are referred to as having DBA syndrome “currently without phenotype.” While most individuals are diagnosed in the first year of life, diagnosis may be made at any time, including adulthood.
In most cases, DBA syndrome is caused by a mutation in one of the genes that encode the ribosomal proteins. The ribosomal proteins have large and small subunits and most patients with DBA syndrome have mutations that cause a decrease either in the small (RPS) or large ribosomal protein (RPL) subunit component. The scientific community has discovered numerous ribosomal protein gene mutations and most recently, non-ribosomal protein gene mutations. These are very exciting discoveries for the DBA syndrome community, as it has resulted in increased scientific attention to this rare disorder. Advances in whole exome and whole genome sequencing are expected to advance additional gene mutation discoveries.
Potentially, patients with DBA syndrome can live long and healthy lives with appropriate medical treatment. The two most common treatments are chronic red blood cell transfusions with chelation therapy and long-term corticosteroid therapy. Some patients experience clinical remission, in which the bone marrow starts to make red blood cells and medical treatment related to the anemia of DBA syndrome is no longer needed. Other patients with DBA syndrome may choose to undergo a stem cell transplant (also called bone marrow transplant or cord blood transplant). This procedure can cure the anemia, but the patients still have DBA syndrome.
About half of the patients with DBA syndrome will have birth defects such as abnormalities of the face, heart, or kidneys. Patients may also have short stature in comparison to their siblings or others their own age without DBA syndrome. In addition, DBA syndrome patients have an increased risk of being diagnosed with cancer at earlier ages than typically seen in those without DBA syndrome.
Diamond Blackfan Anemia syndrome is the preferred name for this disorder, but other names for DBA syndrome include:
Diamond Blackfan Anemia
Blackfan Diamond syndrome
Congenital pure red cell aplasia
Congenital hypoplastic anemia
Aase syndrome (felt to be a subset of DBA syndrome in which there is a finger-like thumb, and not a distinct disorder)
Friends of DBA takes great pride in endorsing the DBA Foundation and the charitable endeavors it funds.
The unwavering support of our families has allowed the Friends of DBA to finance several significant research initiatives. In addition to funds given here in the US, these international grants have supported research in England, France, Sweden, and Italy. The National Heart, Lung, and Blood Institute thankfully started a program to encourage research on the molecular mechanisms underlying DBA and related bone marrow failure syndromes in 2004. This scheme offered a way to guarantee funding for DBA research in spite of the fierce competition for federal research funds. This assistance, together with research funding from the Daniella Maria Arturi Foundation and the Diamond Blackfan Anemia Foundation, resulted in a time of unparalleled advancement in our knowledge of the molecular foundation for DBA. Consequently, private foundations will probably provide a larger share of the overall funds allocated to DBA research in the near future. Therefore, Friends of DBA needs your help now more than ever in order to sustain current and future research grants.
Since the present financial crisis is impacting both public and private businesses, as well as many sectors of our economy, financing for almost all forms of research is probably going to suffer. The National Institutes of Health have had very limited funding in recent years. The National Heart, Lung, and Blood Institute thankfully started a program to encourage research on the molecular mechanisms underlying DBA and related bone marrow failure syndromes in 2004. This scheme offered a way to guarantee funding for DBA research in spite of the fierce competition for federal research funds. This assistance, together with research funding from the Daniella Maria Arturi Foundation and the Diamond Blackfan Anemia Foundation, resulted in a time of unparalleled advancement in our knowledge of the molecular foundation for DBA. But for the following years, it's questionable if the federal government will be able to maintain this level of funding for DBA research. Consequently, private foundations will probably provide a larger share of the overall funds allocated to DBA research in the near future. Therefore, the DBA Foundation needs your help now more than ever in order to sustain the momentum of the previous four years toward understanding the molecular foundation underlying DBA and, more critically, to start translating these findings into effective therapies for children with DBA.
RESEARCH SUPPORT HIGHLIGHTS
Early support for the DBA registry
Support for clinical studies on DBA diagnosis, management, and treatment
Support for the identification of DBA genes
Support for studies on the role of ribosome synthesis defects in the pathophysiology of DBA
Support for the creation of a zebrafish model of DBA
Support for the creation of a mouse model
"DBA has affected our lives in ways we could have never imagined. It has introduced us to the most amazing people – from the dedicated doctors to the wonderful families who are also dealing with DBA. They all exemplify the power of the human spirit and our family."
DIAGNOSIS
Diagnostic criteria for Diamond Blackfan Anemia taken from the International Clinical Care Consensus Document (2008):
Age less than 1 year
Macrocytic anemia with no other significant cytopenias
Reticulocytopenia
Normal marrow cellularity with a paucity of red cell precursors
Near normal but variable neutrophil and/or platelet counts
Supporting criteria:
Major
Gene mutation described in “classical” DBA
Positive family history
Minor
Elevated erythrocyte adenosine deaminase activity
Congenital anomalies are described in “classical” DBA (Congenital anomalies mainly involve the head, upper limbs, heart, and genitourinary system.)
Elevated HbF (fetal hemoglobin)
No evidence of another inherited bone marrow failure syndrome
The above diagnostic criteria define what is termed “classical” DBA, but DBA may also be present in “nonclassical” ways. For example, individuals may present at an age greater than one year, only with congenital anomalies, without anemia, or with a mild hematological phenotype (macrocytosis only). These cases of ‘‘non-classical’’ DBA need to be more carefully identified, particularly when reproductive choices and transplant donor decisions are being made. Furthermore, as the risk of malignancy and other complications of DBA are better defined, the necessity of making a diagnosis in ‘‘asymptomatic’’ individuals will become more important.
There are over 800 patients with DBA syndrome enrolled in the DBA Registry of North America (DBAR). This is a database of patients with DBA syndrome in the United States, Canada, and Mexico. The incidence is estimated at 5-10 cases for every million live births, with an estimated 20-40 new cases per year in the United States and Canada. DBA syndrome is an equal opportunity syndrome, affecting males and females as well as all ethnicities equally. Most patients (~90%) are diagnosed with DBA syndrome during the first year of life; however, some will be diagnosed in later childhood, adolescence, or even adulthood.
According to the DBAR, the average age of presentation of anemia is 2 months and the average age of diagnosis with DBA syndrome is 4 months. Patients with DBA syndrome typically present with common symptoms of anemia including pale skin, sleepiness, irritability, rapid heartbeat, and heart murmurs.
There are several tests to aid in diagnosing DBA.
Complete Blood Count (CBC): This test determines the concentration and composition of cellular components of blood. Values for the number of red blood cells, white blood cells, and platelets in a blood sample are included in the CBC. A CBC may be ordered with “differential,” which measures the number of each type of white blood cell, such as neutrophils (ANC). Blood is typically drawn from a vein. In an infant or young child, blood may also be taken from the heel, toe, or finger. A CBC measures many things, including the following values, which are generally relevant to the DBA patient:
Number of red blood cells
Total amount of hemoglobin in the blood
Fraction of the blood composed of red blood cells (hematocrit)
The size of the red blood cells is referred to as the mean corpuscular volume (MCV)
Number of white blood cells and the percentage of each cell type present (percentage included in CBC with differential only)
Number and size of platelets
Other information about the red blood cells, including the mean corpuscular hemoglobin (MCH) and mean corpuscular hemoglobin concentration (MCHC)
MCV: The mean corpuscular volume (MCV) is a measure of the size of the red blood cells. Patients with DBA tend to have larger than normal red blood cells (macrocytosis). The MCV is measured during a standard CBC.
Reticulocyte Count (Retic): The retic count is the number of immature or young red blood cells. In mathematic terms, immature RBCs/Total RBCs x 100% = retic % count. The reticulocyte % count is a good measure of bone marrow activity, as it quantifies the production of red blood cells within the past 1-2 days. Without medication or being in remission, DBA patients typically have no or extremely low reticulocyte counts (less than 1%). The normal reticulocyte count in healthy individuals, with a normal number of RBCs, is 1 to 2%.
eADA Levels: This test measures the erythrocyte adenosine deaminase (eADA) activity in the blood. Elevated eADA levels are present in approximately 80–85% of patients with DBA. This test must be performed on a sample of the patient’s own blood, meaning it should not be conducted if the patient has had a transfusion in the previous 3 months.
Fetal Hemoglobin Levels: In utero, the fetus makes two kinds of hemoglobin: fetal hemoglobin (sometimes called Hemoglobin F) and adult hemoglobin (sometimes called Hemoglobin A). At birth, the majority of the hemoglobin present is fetal hemoglobin. During the first year of life, the percentage of fetal hemoglobin drops to less than 5% in most healthy individuals, and the percentage of adult hemoglobin rises to 95-100%. However, many patients with DBA maintain an increased level of fetal hemoglobin. The fetal hemoglobin test can be confusing after a patient has had a transfusion, but it still may be possible to run this test.
Bone Marrow Aspiration and/or Bone Marrow Biopsy: A bone marrow examination is a test in which a small amount of bone marrow is removed, usually from the hip bone. A bone marrow aspiration removes only the liquid marrow, whereas a bone marrow biopsy also removes a very small piece of the bone. Pediatric patients typically receive sedation or anesthesia during this procedure. Once removed, the sample is then analyzed to determine how many blood cells of each type (red blood cells, white blood cells, and platelets) are being produced by the bone marrow, as well as the health of the cells. The genetic makeup and physical architecture of the bone marrow can also be determined. The bone marrow in a patient with DBA typically reveals very few early red blood cells (reticulocytes). This test is typically recommended at the time of diagnosis, except for infants, who may delay this test just prior to starting steroids.
Genetic Testing: To date, approximately 70% of DBA patients have a single mutation or deletion in a gene encoding a ribosomal protein. A small percentage of patients have been identified with non-ribosomal protein gene mutations in GATA1, TSR2, and HEATR3. A genetic mutation has not yet been found in approximately 20–25% of patients with DBA. Genetic testing is conducted through a blood test, which typically analyzes DNA found in white blood cells. Therefore, even if a DBA patient has recently had a red blood cell transfusion, the patient’s DNA will be in the patient’s own white blood cells, which can be tested. See the Genetics section for more information on the genetic mutations that are known and suspected to be associated with DBA.
TYPES OF TREATMENT
One type of treatment that might be recommended for someone with DBA is blood transfusions. Blood transfusions might be recommended just as needed when the hemoglobin is lower than normal or as part of a chronic blood transfusion program. Chronic blood transfusions consist of scheduled blood transfusions every 3-6 weeks to maintain the hemoglobin level in a safe range. A DBA patient normally makes his or her own white blood cells and platelets and, therefore, would only require a transfusion of red blood cells.
Blood transfusions are typically given in a hospital setting. Before a transfusion, a small amount of blood will be drawn from the patient for “typing and screening.” Typing refers to the type of blood the patient has (A, B, AB, or O) and screening refers to identifying whether certain antibodies are present. Generally, people must receive blood of their same type to avoid severe transfusion reactions. These tests are followed by the compatibility testing (cross-match). This test ensures that no antibodies are detected in the recipient’s serum that will react with the donor’s red blood cells. Generally, when patients receive a blood transfusion, they receive blood that has been donated from the general population. In the United States, the blood supply is considered to be safe. The federal Food and Drug Administration (“FDA”) is responsible for ensuring the safety of the blood industry in the United States.
STEM CELL TRANSPLANT
Another type of treatment for DBA is to undergo a stem cell transplant. Stem cell transplants (“SCT”) are also known as bone marrow, cord blood, or peripheral blood stem cell transplantation (depending on the donor source). A SCT involves replacing a DBA patient’s unhealthy bone marrow with healthy cells from a donor. The donor’s stem cells can be obtained from bone marrow, peripheral blood, or cord blood. This is a complicated medical procedure that requires several months in the hospital and is not without risk. The reward for a successful bone marrow transplant is that the patient’s bone marrow will function normally, and the patient will not need chronic blood transfusion therapy or corticosteroid medication.
Stem cell transplantation (SCT) is a potentially curative but dangerous procedure. The role of transplantation for patients with DBA remains complex and controversial. In general, whether steroid-responsive or transfusion-dependent, patients with DBA may be considered for transplant before the age of ten years, and preferably between the ages of 2 and 5 years, if an HLA-matched related donor is available. As of the last published analysis, most sibling transplants used chemotherapy alone as a conditioning regimen, while most of the alternative donor (mismatched family or unrelated donor) transplants used a combination of chemotherapy with radiation therapy for pre-transplant conditioning. Data from the DBAR show overall survival of 77% for allogeneic sibling SCT (94% for allogeneic sibling SCT age nine years and less) and 36% for alternative donor SCT (86% for alternative SCT done after 2000).